What is it:
Gluten is a protein, belonging to a family of proteins known as prolamins.
Where does it come from:
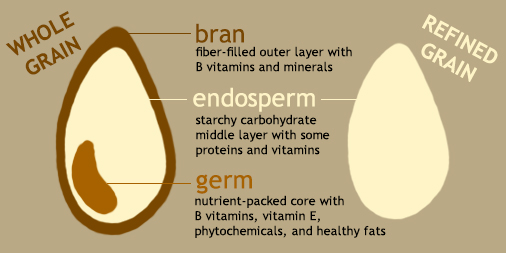
Prolamins are found in the endosperm of cereal grains such as wheat, barley and rye – see figure 1 below. In wheat the prolamins are called gliadins and glutenins, in barley they are called hordeins and in rye, secalins1.
Figure 1: Diagrammatic representation of a cereal grain
What does it do:
The biological function of prolamins is to provide nutrients for germination and growth of the cereal seedlings2. Whilst some cereal growers may save a proportion of the harvested grain for planting the following year, the bulk of the crop will be farmed and processed for human consumption.
This YouTube video shows how wheat grain is milled to produce flour.
The milling of cereal grains is probably one of the oldest industrial processes we know. Nowadays different grain varieties and blends, coupled with an array of milling techniques, provide the customer with flours suitable for a multitude of end products e.g. bread, pizza, pasta, cakes, biscuits.
Bread-making typically involves mixing flour, water and yeast. These ingredients are kneaded to give a smooth elastic dough which is allowed to rise/prove before it is baked. The gliadin and glutenin proteins in the flour form chemical bonds during kneading to create gluten, giving the dough its strength and elasticity3. Carbon dioxide given off by the yeast in the rising/proving process is trapped by the gluten network and this ‘airy’ matrix is supported during baking to give a light and fluffy loaf of bread.
Coeliac Disease and gluten sensitivity
Most people can consume gluten without any apparent ill-effects. Twenty or so years ago it was thought that a small proportion of the population confirmed to be suffering from coeliac disease (CD) should adopt a gluten-free diet4. Whilst currently 1% of the UK population have been diagnosed with CD5, CoeliacUK state there are many more people affected by CD who have had no formal diagnosis. This is because symptoms can often be attributed to other gastro-intestinal disorders such as irritable bowel syndrome.
CD is an autoimmune* condition whose symptoms include bloating and abdominal pain. More seriously this can lead to fatigue, weight loss and malnutrition due to damage sustained by the lining of the small intestine (see figures 2 and 3) and the resulting malabsorption of nutrients.
*The body’s immune system attacks its own healthy tissue
Figure 2: Healthy small intestine lining
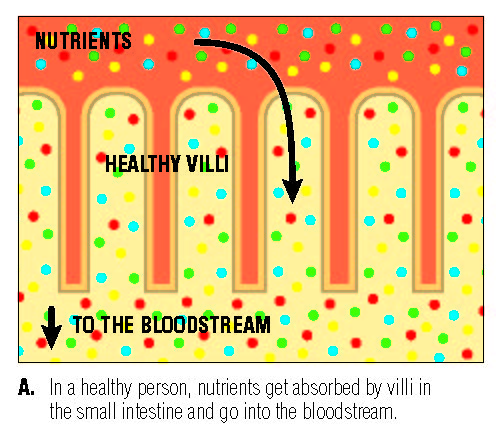
Figure 3: Small intestine lining damaged due to Coeliac Disease
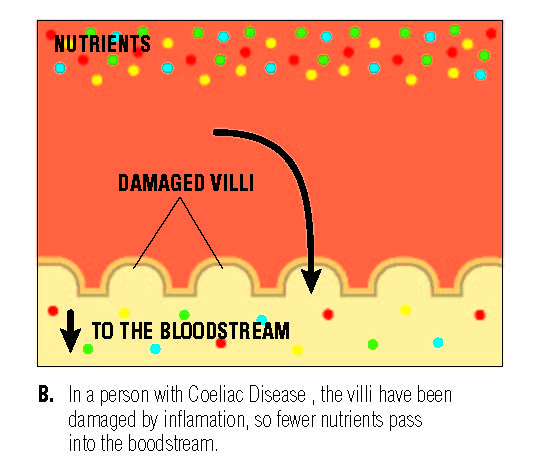
Looking back to the post on ‘Polypeptides and Protein’ we recall proteins are composed of long chains or groups of sub-units called amino acids. Prolamins contain an abundance of the amino acids proline and glutamine1,4 which can be resistant to digestion in the human gut1. It is these longer chains of amino acids which have escaped complete digestion that are attacked by the immune system as if they were foreign invaders, at the same time causing inflammation and damage to the lining of the small intestine6 as seen in figure 3.
Non-coeliac gluten sensitivity is where symptoms similar to CD are experienced but CD is ruled out following negative testing prescribed by a GP or other health physician. CoeliacUK report that since this is a fairly new area of research there are no tests available to confirm non-coeliac gluten sensitivity. The only option may be to exclude all gluten-containing foods from the diet to see if symptoms are alleviated.
A gluten-free diet
There is no cure for CD which must be controlled with a gluten-free diet. Whilst there are many healthy foods which someone with CD can eat, for example, fresh meat, fresh fish, milk, eggs, cheese, vegetables and fruit, all foodstuffs containing wheat, barley and rye should be avoided. This will include obvious flour-based products like bread, pizza, pasta, cakes and biscuits, but also the not so obvious choices like battered fish, meats containing cereal bulking agents, beer, stout, malt vinegar, gravy and sauce thickenings, some confectionary and ice creams and other products where contamination during processing is possible, such as porridge oats. If in doubt look at food labels for allergens, which must be highlighted by law – see the post ‘Setting Standards’.
For more information on CD and a gluten-free diet, check out CoeliacUK linked here
References
- COMINO, I., MORENO, M., REAL, A., RODRÍGUEZ-HERRERA, A., BARRO, F., SOUSA, C. The gluten-free diet: testing alternative cereals tolerated by celiac patients. Nutrients, 5(10), October 2013, 4250–4268. Available from: https://doi.org/10.3390/nu5104250
- WUJUN, M.A., YU, Z., SHE, M., ZHAO, Y., ISLAM, S. Wheat gluten protein and its impacts on wheat processing quality. Front. Agr. Sci. Eng., 2019, 6(3): 279‒287. Available from: https://doi.org/10.15302/J-FASE-2019267
- DELCOUR and HOSENEY, 2010; KIEFFER, 2006, In: Gluten Chemistry and Functionality. Food Science Toolbox. Available from: https://cwsimons.com/gluten-chemistry-and-functionality/
- STEINMARK, I.E., ed. Magnificent Molecules: Gluten. Royal Society of Chemistry. May 2016. Available from: https://edu.rsc.org/magnificent-molecules/gluten/2000021.article
- Coeliac Disease – Overview. NHS, 2019. Available from: https://www.nhs.uk/conditions/coeliac-disease/
- HILL, M., ed. Attack of the Gluten. American Chemical Society. February 2012. Available from: https://www.acs.org/content/acs/en/education/resources/highschool/chemmatters/past-issues/archive-2011-2012/gluten.html