How the brain controls appetite
Nutrients in food provide energy for daily living, sustain growth during pregnancy and in childhood, support tissue maintenance, keep the immune system healthy and help regulate chemical reactions within the body. If we’re making conscious decisions about keeping our bodies in good shape our food choices will be based on healthy eating guidelines, so presumably there isn’t a packet of crisps, a cream cake or a biscuit in sight, ever? Right?
Wrong? It just doesn’t work like that does it! But why?
The drive to eat isn’t always about rational choice. Nor does it necessarily stem from hunger or a need for sustenance. Wanting or desire can be related to an appetite or ‘need’ for a particular food item. Indeed the sensory properties of food – its appearance, smell, flavour, texture – can cajole us into eating when we are not hungry, or to carry on eating when full.
Early research around appetite regulation by physiologists such as Claude Bernard (1813-1878) and Walter Cannon (1871-1945) centred mainly on behavioural homeostatic machinery, whereby signals within the body stimulate and subsequently suppress the desire to eat1.
Knowledge of how these mechanisms operate has increased substantially since Bernard and Cannon and a very brief overview is provided.
Homeostatic regulation of appetite
Complex neural pathways modulate energy balance in the human body, involving the following sensations:
hunger – a strong desire to eat
appetite – a desire to eat, sometimes due to hunger
satiation – the desire to eat has been satisfied
satiety – the desire to eat is absent
Figure 1: Schematic representation showing the brain, specifically the arcuate nucleus at the base of the hypothalamus, gut and adipose tissue (fat cells), all of which are involved in key homeostatic regulation pathways
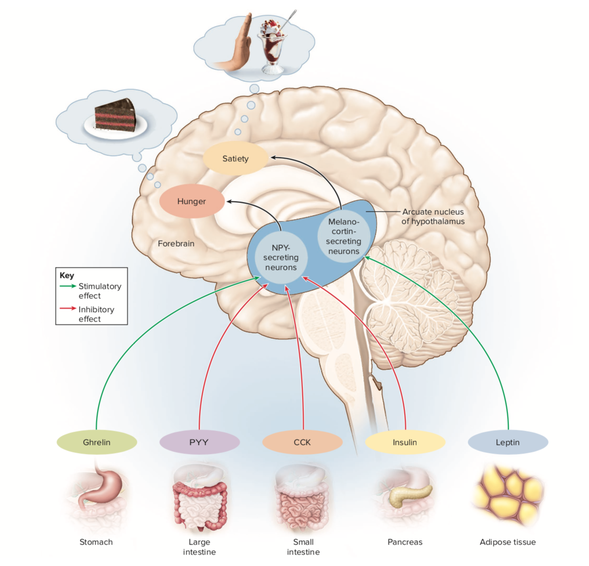
Source: quora.com – Ken Saladin – Appetite regulating hormones
When stimulated, the arcuate nucleus expresses orexigenic peptides (e.g. neuropeptide Y or NPY) to increase appetite and anorexigenic peptides (e.g. alpha melanocyte stimulating hormone or aMSH) to decrease appetite. These peptides are sequences of amino acids (see the post ‘Polypeptides and Protein’) produced by neurons in the brain and are known as neuropeptides.
Whether the arcuate nucleus signals for an increase or decrease in feeding will be dependent on the stimuli it receives from the gut and adipose tissue. A brief summary of the activity of the hormones ghrelin, PYY, CCK, insulin and leptin shown in Figure 1 is given below1. There are also other hormones, neuropeptides, mechanical and chemical signals involved in the homeostatic regulation of food intake not covered here.
Ghrelin the ‘hunger’ hormone, is synthesized primarily within cells lining the stomach. There are sharp peaks in the levels of ghrelin circulating prior to eating, which fall off after feeding – see Figure 2.
Figure 2: Averaged plasma ghrelin concentrations for 10 humans over a 24 hour period
CCK, or cholecystokinin, is a hormone released from the small intestine in response to the ingestion of fats and proteins and is a mediator of satiation.
PYY, or Peptid YY, is produced by cells in the intestine and induces post-meal satiety. Circulating levels of PYY peak 1-2 hours after a meal.
Insulin is a hormone secreted by the pancreas in response to increasing concentrations of glucose in the blood following carbohydrate digestion. It acts as an anorectic signal in the brain to decrease food intake. Levels of insulin in the blood rise rapidly after a meal and are relative to the sensitivity of the cells which insulin targets for glucose uptake and/or storage; in particular, muscle cells which use glucose for energy and adipose tissue where excess glucose is converted to fat.
Leptin is a key hormone produced by adipose tissue. Regarded as a long-term regulator of energy balance, circulating levels of leptin correlate with the amount of adipose tissue in the body. If an individual gains body fat, more leptin is secreted which in turn leads the brain to signal for a reduction in food intake. Conversely, a reduction in adipose tissue will cause a reduction in circulating leptin and appetite will be stimulated.
Obesity leads to increased amounts of leptin in the blood, but it seems leptin resistance (reduced sensitivity of receptors in the brain) is responsible for a decrease in efficacy of the hormone to counteract weight gain.
Research tells us that homeostatic appetite control is only one of a number of systems active within the nonconscious areas of the brain which attempt to control when, why and what we eat. Another is hedonic control of appetite and whilst homeostatic and hedonic control can be depicted as separate entities, they do interact functionally.
Hedonic eating
The motivation to eat for pleasure rather than due to hunger is known as hedonic eating and the relationship between the obesity epidemic, hedonic eating and by association ultra-processed, highly palatable foodstuffs is clear2. This has concentrated research interest in areas of overeating and appetite control, with particular focus on cues from the external environment and how hedonic appetite is implicated.
Over the last 50 years, changes in agriculture practices have led to an expansion of food availability and diversity. Yet a 2016 report from The Food Foundation3 states that despite the average UK family having lots of dietary options, 50.4% of the food purchased by a typical UK family is ultra-processed.
“The term ‘ultra-processed’ was coined to refer to industrial formulations manufactured from substances derived from foods or synthesised from other organic sources. They typically contain little or no whole foods, are ready-to-consume or heat up, and are fatty, salty or sugary and depleted in dietary fibre, protein, various micronutrients and other bioactive compounds. Examples include: sweet, fatty or salty packaged snack products, ice cream, sugar-sweetened beverages, chocolates, confectionery, French fries, burgers and hot dogs, and poultry and fish nuggets.” (Foresight report on Food Systems and Diets: Facing the Challenges of the 21st Century, September 2016, Global Panel on Agriculture and Food Systems for Nutrition4)
The high palatability provided by ultra-processed foods is relayed to the reward circuits in the brain leading to an upregulation in dopamine, endocannabinoids and opiates. These neurotransmitters are responsible for ensuring the compulsion to eat is maintained by increasing expression of the homeostatic ‘hunger’ neuropeptides such as NPY and blocking the effect of the satiety inducing hormones such as insulin, leptin and CCK1, all detailed above.
Dopamine is regarded as the ‘learning’ chemical, in so much once encountered we learn from the pleasurable experience and become motivated to repeat it5. One such reason why we still have room for dessert after a generous main course; knowing the dessert is probably not nutritious but desiring it all the same.
Keeping the brain reward centres in check
How do we do this and avoid eating calorie laden, high fat, high sugar foods on a regular basis? It’s not an easy task, given we’re taking on the might of our irrational, impulsive, nonconscious brain in an environment laden with desirable, ultra-processed foodstuffs.
Tips
- Plan meals in advance and shop according to the plan
- Avoid shopping for food when hungry
- Avoid buying ultra-processed foods – my guess is you will know the ones you find difficult to resist
- Be aware of the cues which drive you to seek out ultra-processed foods, so these situations can be moderated or avoided altogether
- Eat foods that send strong satiety signals to the brain, for example protein, whole grains, vegetables and fruit
- If you need to snack, eat a portion of fruit or a few unsalted nuts
References
- HOPKINS, M., BLUNDELL, J., HALFORD, J. et al. The Regulation of Food Intake in Humans. [Updated 2016]. In: FEINGOLD, K.R., ANAWALT, B., BOYCE, A. et al., editors. Endotext [Online]. South Dartford (MA): MDtext.com, Inc. 2000-. [Viewed 7 May 2021]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278931/
- RIBEIRO, G. et al. Association between hedonic hunger and body-mass index versus obesity status. Scientific Reports [Online]. Nature. April 2018, 8, 5857. [Viewed 10 May 2021]. Available from: doi.org/10.1038/s41598-018-23988-x
- THE FOOD FOUNDATION. FORCE-FED Does the food system constrict healthy choices for typical British families? 2016. [Viewed 10 May 2021]. Available from: https://foodfoundation.org.uk/wp-content/uploads/2016/07/The-Food-Foundation-64pp-A4-Landscape-Brochure-AW-V32.pdf
- MONTEIRO, C.A. et al. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutrition [Online]. March 2017. [Viewed 10 May 2021]. Available from: doi. 10.1017/S1368980017000234
- WISE, R.A. Dopamine, Learning and Motivation. Nature Reviews Neuroscience [Online]. Nature. June 2004, 5. [Viewed 10 May 2021]. Available from: https://www.researchgate.net/profile/Roy-Wise/publication/8554485_Dopamine_learning_and_motivation/links/0912f511a5977a5753000000/Dopamine-learning-and-motivation.pdf
Hi Jane – Hope you are well. “Wanting or desire can be related to an appetite or ‘need’ for a particular food item. ” …brought with me some fruit to work trying to eat well, but at the 4 pm tea time, couldnt help searching for something with chocolate as I ‘need’ this particular type of food.